27
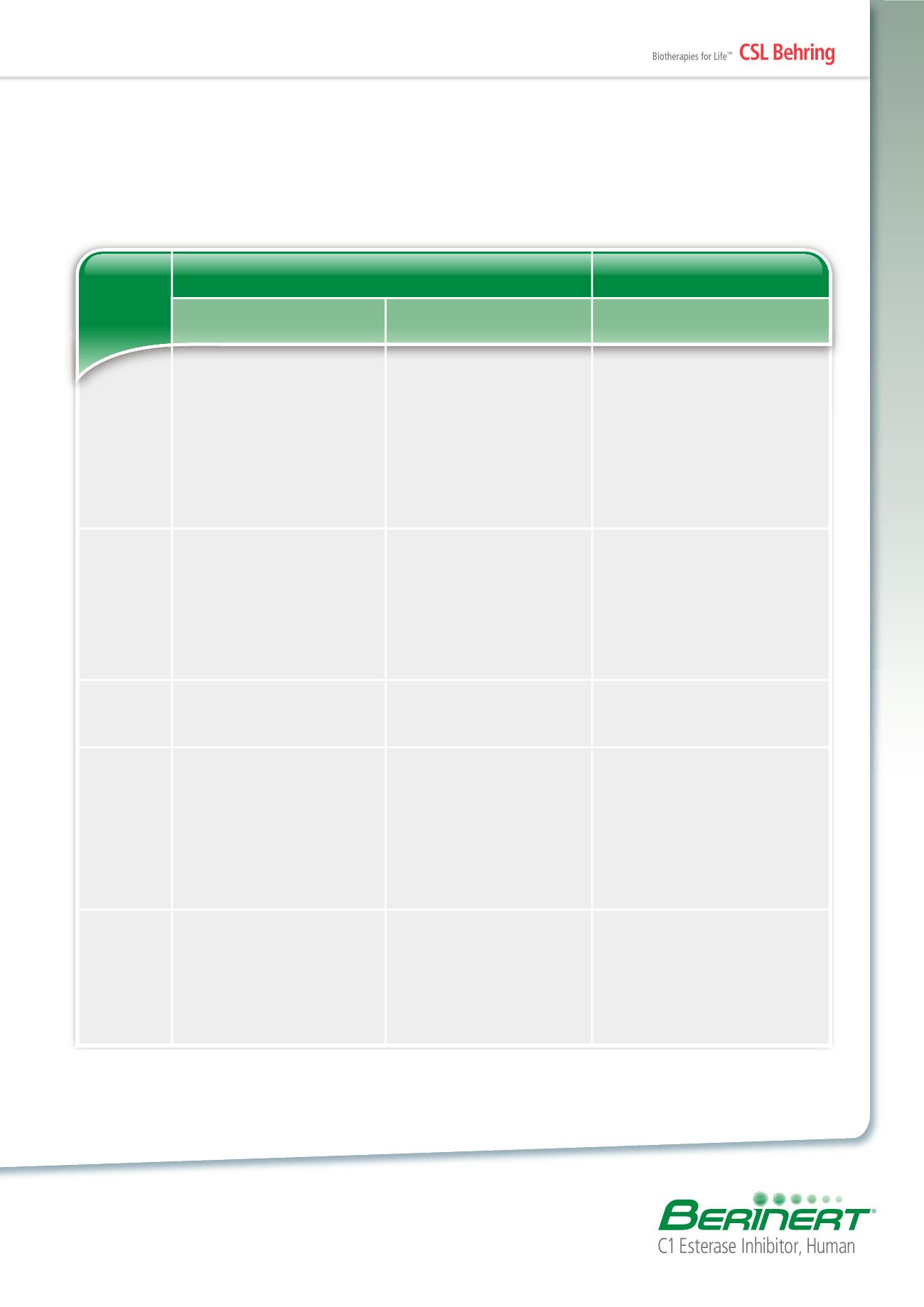
Table 7 – Differential Diagnosis of Hereditary, Allergic, and ACE-inhibitor-related Angioedema
62
History
Triggering
factors
Prodromal
symptoms
Symptoms
Laboratory
investigations
Hereditary Angioedema
(C1-INH Deficiency)
Bradykinin-mediated Angioedema
Histamine-mediated Angioedema
•
Usually positive familial history,
though de novo mutation is possible
•
Usually manifests in the first,
second, or third decade of life
•
No history of urticaria
•
Spasmodic abdominal attacks/colic
•
Increased incidence of autoimmune
diseases
•
Physical trauma or stress,
particularly after dental surgery
•
Emotional stress
•
Infectious diseases
•
Menstruation
•
Estrogen therapy
•
Often no discernible trigger
•
Occurs in 50% of cases
(eg, paresthesias, reticular
erythema, malaise)
•
Subcutaneous angioedema
•
Abdominal pain
•
Acute narrowing of the airway
(laryngeal edema)
•
Low plasma C1-INH activity
•
Low C4
•
Low plasma C1-INH concentration
in HAE-I
•
Normal or increased, but
functionally impaired plasma
C1-INH concentration in HAE-II
Angioedema Associated
With Chronic Urticaria
•
Usually no familial history
•
History of urticaria
•
Typically no abdominal pain
•
Possible allergens, medicines,
physical measures
•
Trigger often unknown
•
None
•
Itching
•
Urticaria
•
Rarely, abdominal pain
•
In rare instances, acute narrowing
of the airway (laryngeal edema)
•
Usually responds to antihistamines
but increased dosing may be
necessary
•
Normal
Angioedema Associated
With ACE Inhibitors
•
No familial history
•
First manifestation usually after
the fourth decade of life
•
Usually occurs shortly after
initiation of ACE inhibitor therapy
•
ACE inhibitors
•
None
•
Subcutaneous angioedema
•
Cough
•
Acute narrowing of the airway
(laryngeal edema)
•
Swelling of the tongue
•
Gastrointestinal symptoms
•
Usually remits when ACE inhibitor
discontinued
•
Normal
HAE
ACE=Angiotensin-converting enzyme; C1-INH=C1 esterase inhibitor.